What Is Lp(a) and Why Doctors Call It the Silent Heart Killer?
Heart disease often feels like something that happens to “other people,” until it doesn’t. The truth is, millions of people are walking around with a hidden risk factor that standard cholesterol tests don’t even measure. It’s called Lp(a) cholesterol, and it quietly raises the chance of heart attack or stroke without any warning signs. This particle has been called the silent heart killer for a reason: it can sneak up on you even if you eat well, exercise, and maintain a healthy weight.
Understanding what it is, how it works, and what you can do about it is one of the most important steps you can take to protect your heart health. Let’s unpack what makes this particle so dangerous and how you can get ahead of it.
What Is Lp(a)?
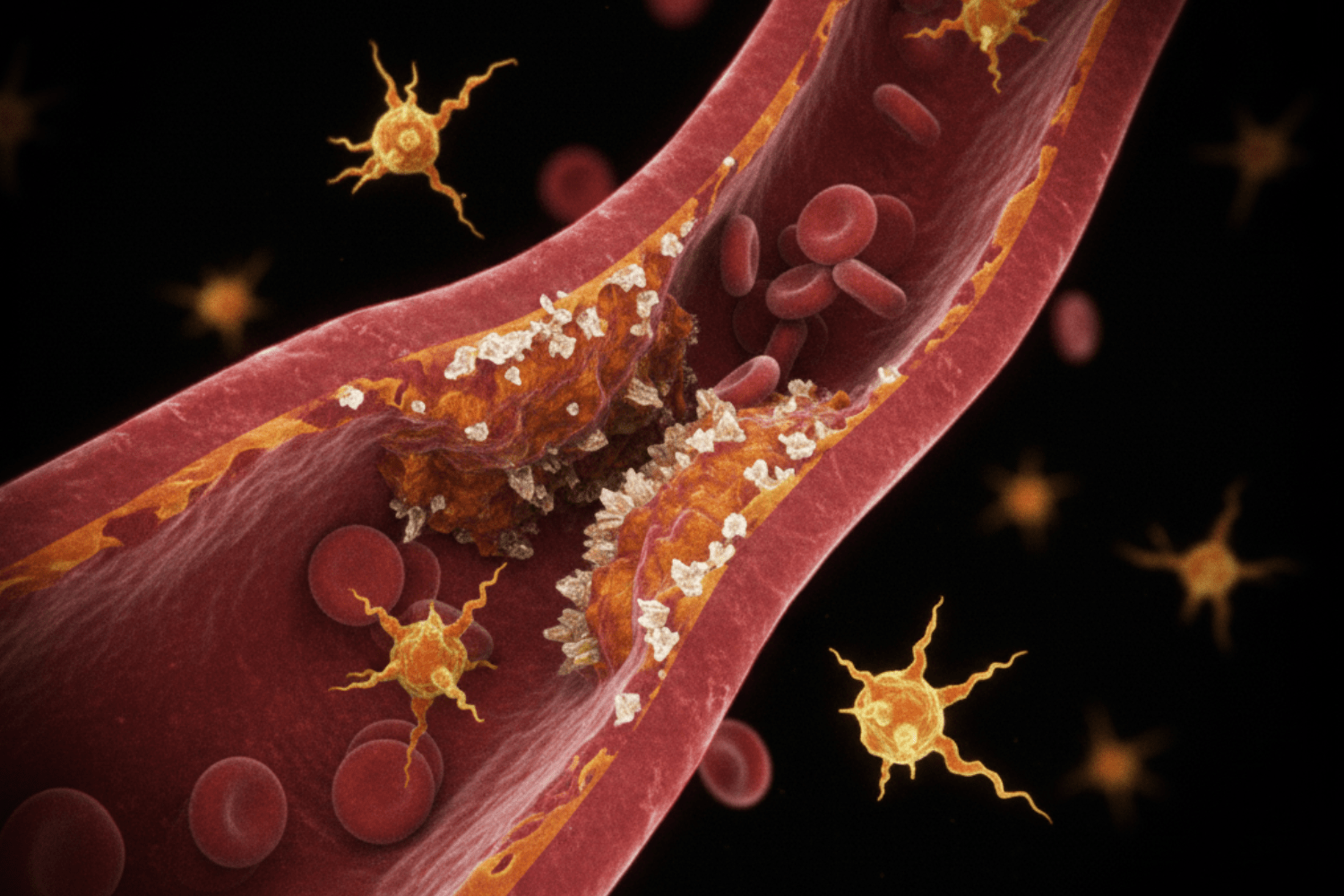
Lp(a), short for lipoprotein(a), is a type of cholesterol-carrying particle that circulates in your blood. At first glance, it looks a lot like LDL, the so-called “bad cholesterol,” but with one crucial difference: it carries a special protein called apolipoprotein(a). That little protein gives Lp(a) unique, and sometimes dangerous, properties.
Here’s what makes it important: high levels of Lp(a) can cause cholesterol and other fatty deposits to stick to the walls of your arteries faster, triggering inflammation and narrowing your blood vessels over time.
Unlike other forms of cholesterol, Lp(a) levels are mostly determined by your genes. You can’t just eat a perfect diet and watch those numbers drop. That’s why many cardiologists want more people to get tested at least once in their life.
Lp(a) Cholesterol and Your Heart
Lp(a) cholesterol acts like a stealthy builder of plaque inside your arteries. You can feel fine one day and then, out of nowhere, suffer a major event such as a heart attack or stroke. This is why doctors refer to it as the silent heart killer.
Research shows that elevated Lp(a) is strongly linked to a higher risk of heart disease, aortic valve narrowing, and blood clots. Think of it like this: while LDL raises your baseline risk, Lp(a) piles on extra danger, especially if you already have other risk factors.
Here are some conditions scientists have tied to high Lp(a):
- Coronary artery disease
- Peripheral artery disease
- Stroke and mini-stroke (TIA)
- Aortic stenosis (narrowing of the heart valve)
Because Lp(a) is not part of standard cholesterol testing, many people never find out they have it until after they’ve had a cardiovascular event. That’s why awareness matters so much.
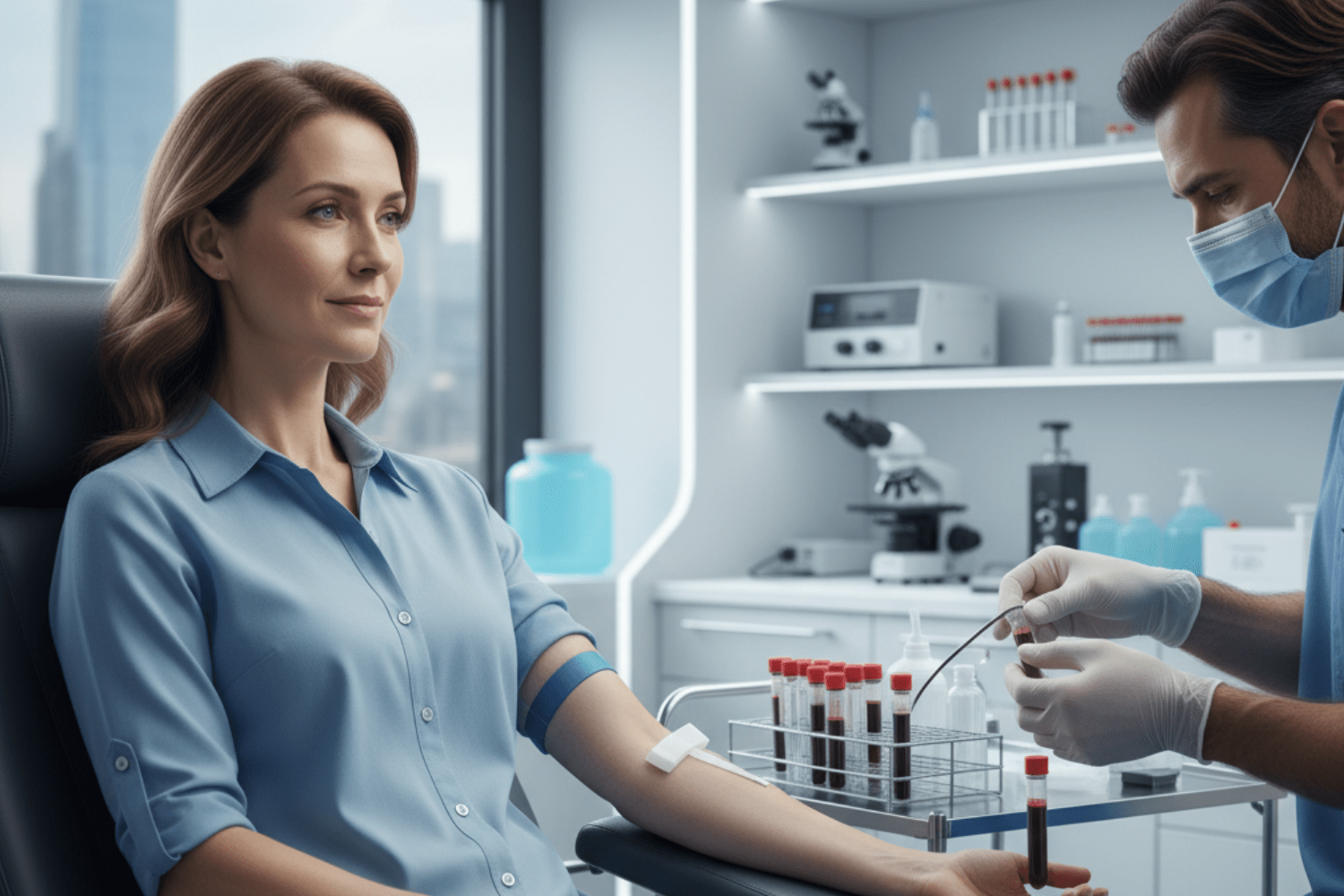
How to Know Your Lp(a) Levels
Finding out your levels is surprisingly simple: it’s just a one-time blood test. Your doctor can order it along with your other cholesterol tests.
Testing is especially important if you:
- Have a family history of premature heart disease
- Have had a heart attack or stroke at a young age
- Have high LDL despite a healthy lifestyle
- Are of African ancestry, since higher levels are more common
Many experts recommend that everyone get tested at least once. If your levels are high, your doctor might monitor you more closely and suggest early action to protect your arteries.
Lp(a) and Cardiovascular Health
When Lp(a) is elevated, it doesn’t just sit quietly in the bloodstream. It can cause ongoing inflammation in the vessel walls, making plaque more unstable and likely to rupture. That’s one reason why heart attacks and strokes linked to Lp(a) can happen suddenly.
Because levels are almost entirely inherited, it’s not something you can completely “fix” through willpower or perfect habits. But knowing you have higher Lp(a) lets you take extra care of your cardiovascular health.
Certain groups are at greater risk:
- People with a parent or sibling who had heart disease before age 55 (men) or 65 (women)
- People of African ancestry, who statistically have higher Lp(a) levels
- People with other cholesterol disorders
Being proactive means you and your doctor can manage every other factor you can control, from blood pressure to LDL cholesterol, to lower your overall risk.
Can You Lower Lp(a)?
People often panic when they learn they have high Lp(a), and the first question is always the same: “Can I bring it down?”
The truth is tricky because your genes set your Lp(a) level; there’s no quick fix. But that doesn’t mean you’re powerless. You can still take steps that protect your heart and lower your overall risk.
Ways to Reduce Lp(a) Naturally
This is one of the most common questions, and the honest answer is tricky. Because Lp(a) is genetic, there isn’t a magic food or exercise that will dramatically lower it. Still, there’s a lot you can do to keep your heart healthy even with elevated levels.
Try focusing on these habits:
- Eat a heart-smart diet: Lots of vegetables, fruits, whole grains, lean proteins, and healthy fats.
- Stay active: Aim for at least 150 minutes of moderate movement a week.
- Stop smoking: Tobacco makes blood vessels sticky and more prone to plaque buildup.
- Keep LDL in check: Lowering LDL can reduce the overall cholesterol that Lp(a) can carry into your arteries.
Some research suggests that niacin supplements can lower Lp(a) a bit, but the evidence is mixed, and it can have side effects. Always talk with a healthcare provider before starting supplements.
High Lp(a) Treatment Options
Right now, there isn’t a widely available drug that dramatically lowers Lp(a), but researchers are working on it. Here’s what doctors currently use to help people with very high levels:
Treatment | What It Does | Effect on Lp(a) |
Lower LDL and overall heart risk | Minimal effect | |
Lower LDL significantly | Reduce Lp(a) by about 20–30% | |
Filters Lp(a) from the blood | Significant but temporary drop |
Several new treatments are in late-stage clinical trials, including therapies that turn down the gene responsible for Lp(a) production. These could be game-changers in the next few years. Until then, the focus is on controlling everything else: blood pressure, blood sugar, weight, and LDL cholesterol.
Conclusion
Knowing about Lp(a) cholesterol could save your life. It’s one of those hidden risk factors that too often flies under the radar until it’s too late. Getting a simple blood test, keeping your heart-healthy habits strong, and staying in touch with your doctor about your overall risk can make all the difference.
Take action now, not later. Ask your doctor about testing, share your family history, and take every small step you can to protect your heart. The more you know, the more power you have to stay healthy for the long run.


